 May is Huntington’s Disease (HD) Awareness Month, sponsored by the Huntington’s Disease Society of America. This often unknown and misunderstood disease and it’s link to Alzheimer’s symptoms is worthy of discussion. Let’s delve into understanding Huntington’s Disease.
May is Huntington’s Disease (HD) Awareness Month, sponsored by the Huntington’s Disease Society of America. This often unknown and misunderstood disease and it’s link to Alzheimer’s symptoms is worthy of discussion. Let’s delve into understanding Huntington’s Disease.
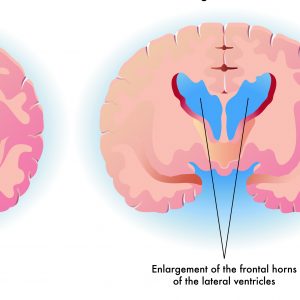
According to the Huntington’s Disease Society of America, HD is a fatal genetic disorder that causes the progressive breakdown of nerve cells in the brain. It deteriorates a person’s physical and mental abilities during their prime working years and has no cure. HD is known as the quintessential family disease because every child of a parent with HD has a 50/50 chance of inheriting the faulty gene. Today, there are approximately 30,000 symptomatic American and more than 200,000 at-risk of inheriting the disease.
Symptoms of HD are described as having ALS, Parkinson’s and Alzheimer’s-simultaneously. Symptoms usually appear between the ages of 30 to 50 and worsen over a 10 to 25-year period. Ultimately, the weakened individual succumbs to pneumonia, heart failure or other complications. Everyone has the gene that causes HD, but only those that inherit the expansion of the gene will develop HD and perhaps pass it on to each of their children. Every person who inherits the expanded HD gene will eventually develop the disease. Over time, HD affects the individual’s ability to reason, walk and speak.
HD Symptom’s include:
- Personality changes, mood swings and depression
- Forgetfulness and impaired judgment
- Unsteady gait and involuntary movements
- Slurred speech, difficulty in swallowing and weight loss
The symptomatic links to Alzheimer’s disease or other forms of dementia include personality changes, mood swings, depression, forgetfulness, and impaired judgment. The complex symptoms of HD are manifested in the changes of motor, cognitive and psychiatric symptoms. These symptoms begin insidiously and progress over many years, until the death of the individual. The average length of survival after clinical diagnosis is typically 10 -20 years, but some people have lived thirty or forty years with the disease. Late stage HD can last up to a decade or more.
Caregivers of persons with Huntington’s Disease need education, support, and resources. State organizations of the Huntington’s Disease of America provide a means for caregivers and persons living with HD to come together. I’ve been honored to speak at several of the Texas conferences and I will tell you that learning about this disease and the challenges they face has enlightened me to the fact that awareness of this disease is greatly needed by society. I encourage our readers to join the HDSA social media campaign #LetsTalkAboutHD.
Like Alzheimer’s, families of persons with HD need tools to cope, a great understanding of their challenges, and a greater sense of empathy.
Pam Brandon is President/Founder of AGE-u-cate® Training Institute and a passionate advocate for older adults and those who serve them. She is the creator of the Dementia Live® sensitivity awareness program to help caregivers and the community understand what it’s like to live with cognitive challenges.
 March 3 -7 is Careers in Aging Week and an appropriate time to talk about the importance of this topic. No longer are the shortages of direct care staff and others in long term care a subject of the future. The crisis is looming and it is serious.
March 3 -7 is Careers in Aging Week and an appropriate time to talk about the importance of this topic. No longer are the shortages of direct care staff and others in long term care a subject of the future. The crisis is looming and it is serious. More than 5.5 million people across the United States are living with Alzheimer’s disease and other forms of dementia. As the baby boom generation ages, the numbers are projected to grow at alarming rates. Although state dementia training requirements vary greatly, overall requirements are expanding for certified nursing assistants, administrators, licensed practical nurses, health aides, personal care assistants and law enforcement and emergency personnel.
More than 5.5 million people across the United States are living with Alzheimer’s disease and other forms of dementia. As the baby boom generation ages, the numbers are projected to grow at alarming rates. Although state dementia training requirements vary greatly, overall requirements are expanding for certified nursing assistants, administrators, licensed practical nurses, health aides, personal care assistants and law enforcement and emergency personnel. Stress Reaction is a term being used more often to describe communication in persons living with dementia. Behavioral expression, too, is communication. In a growing number of circles, the term behavioral expression is being replaced by stress reaction simply because behaviors sometimes leans toward being a negative descriptive of how persons with dementia express unmet needs.
Stress Reaction is a term being used more often to describe communication in persons living with dementia. Behavioral expression, too, is communication. In a growing number of circles, the term behavioral expression is being replaced by stress reaction simply because behaviors sometimes leans toward being a negative descriptive of how persons with dementia express unmet needs.