As a parent or caregiver, you likely have been asked, “When is dinner?” or “Do I have to do that now?” Sometimes the questions are perpetual and never ending. We are living moment to moment, but there is always a feeling of what is next. If you have been a caregiver for someone with Alzheimer’s disease, there is another challenge of living in the present while thinking about the past.
Emotions and Memories
People with Alzheimer’s disease or other dementias retain their long-term memories, especially ones that are tied to emotion. The progression of Alzheimer’s disease varies with each person. However, those with this disease typically remember people and events from the past.
If you have worked with and cared for someone with dementia, you have likely heard questions about a long-lost relative, or an important event that happened long ago. It is painful to see someone you care for express their sadness or longing for someone or something that is long gone. When these questions or feelings emerge while you are trying to get something done for and with the person, it is even more challenging.
Living in the Now and in the Past
How do you do what needs to be done, while acknowledging the feelings of loved ones? How do you live in the perpetual now, with all that needs to be done? What is the best approach for taking care of loved ones with dementia while taking care of everything else?
Acknowledge the emotions and memories of your loved one. Try to understand that people with Alzheimer’s disease may find security in memories. The feelings remain intact. Honor those feelings. Live in that moment, even though it is in the past. Even though you may have heard the same feelings and stories many times before.
Determine how you can help that person do what needs to be done. Consider whether or not what needs to be done can be modified. Also try to delay the activity if possible. Reach out to other care partners to find other strategies.
Taking Care of Emotions and Business
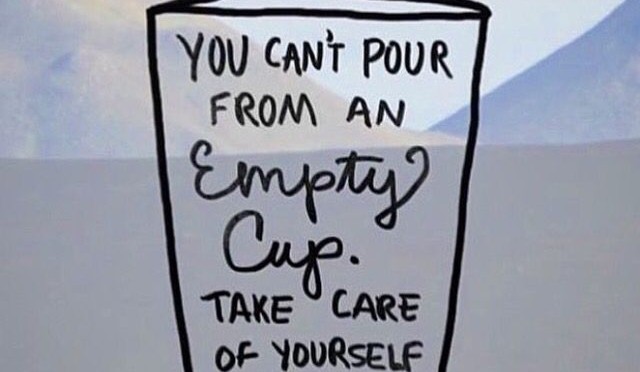
It is hard, sometimes impossible, to live in the perpetual now, with all that needs to be done. Caring for someone with dementia who is likely living in the past is difficult, especially with the pressure of getting things done. Putting their feelings first helps to live in the now, focusing on where they are. Remember that you are doing your best. Take care of yourself and know that your work is valuable.
Kathy Dreyer, Ph.D., is an Advisor at AGE-u-cate® Training Institute, which develops and delivers innovative research-based aging and dementia training programs such as Dementia Live® and Compassionate Touch®, for professional and family caregivers; kathy.dreyer@ageucate.com